Posted: January 23rd, 2017 | Author: DoseSpot | Filed under: Basics, Controlled Substances | Tags: CMS, Controlled Substances, DEA, e-Prescribing, e-Prescribing controlled substances, e-Prescribing Integration, EPCS, health IT, healthcare IT, Maine State Mandate, meaningful use, Opioid Epidemic, State Mandates, surescripts | No Comments »

Navigating the waters of e-Prescribing can seem like a very daunting task considering the various state and federal regulations. To assist you in understanding, let’s review the information relative to e-Prescribing of Controlled Substances (EPCS) in all 50 states and how your state is measuring up.
Until recently, one-half of all U.S. States prohibited e-Prescribing of controlled substances. The thought was that paper prescriptions were safer and more secure. On September 15, 2015, however, Vermont became the last state to allow electronic prescribing of controlled substances, or Schedule II-V medications, making this process legal in all 50 U.S. states.
“We certainly believe that because of the enhanced security associated with e-Prescribing of controlled substances, the opportunity for abuse, misuse, and fraudulent activity is going to be dramatically reduced,” said Ken Whittemore, BSPharm, MBA, Senior Vice President of Professional and Regulatory Affairs at Surescriptsâ„¢, a nationwide health information network.
With this process now legal in all 50 states, and the safer option at that, it may be surprising to find that as of the most recent data available, only 7% of prescribers are sending controlled substances on the Surescripts network.
So, why the discrepancy? Are pharmacies not accepting electronic prescriptions? Are prescribers not able, or willing, to send these prescriptions electronically? Is this process too difficult? Why is this process used in some states so heavily, but so infrequently in others?
Pharmacies are ready!
In 2010, the DEA published a final ruling giving not only practitioners the option to write controlled substances electronically, but also for pharmacies to receive, dispense, and archive electronic prescriptions.
“It became incumbent upon a number of stakeholder groups in the pharmacy industry to tackle the issue and bring states into alignment with the DEA’s rule,” Ken Whittemore, BSPharm, MBA told Pharmacy Today.
Many pharmacy stakeholder groups, including APhA, the National Alliance of State Pharmacy Associations (NASPA), the National Association of Chain Drug Stores, and Surescripts, worked together over a 5-year period to rework some state laws, a process that can take a long time. Between 2010 and 2015, the pharmacy end of the spectrum worked hard on adoption and enablement, while prescriber enablement trailed. Using data from Surescripts, a study published in the January 2015 American Journal of Managed Care found that pharmacies with technology in place to accept e-Prescriptions for controlled substances increased from 13% in 2012 to 30% in 2013. By contrast, only 1% of all prescribers were capable of e-Prescribing controlled substances in 2013.
However, between 2012 and 2013, the number of e-Prescriptions for controlled substances grew dramatically from 1,535 to 52,423. Talk about a rapid jump!
According to the 2015Â Surescripts National Progress Report, an average of 81% of pharmacies were enabled for EPCS in 2015. States including Hawaii and Mississippi were at the bottom of this list with less than 70% of pharmacies enabled, while states in the Northeast such as Massachusetts, New York, New Hampshire, and Rhode Island led this list with over 90% of pharmacies enabled for EPCS.
As of December 1, 2016, these numbers have only risen, with both Hawaii and Mississippi now having over 75% of pharmacies enabled. New York and Maine lead the race on that front with 96.8% and 95.2% of pharmacies enabled currently. This is in large part due to the state mandates put into place in 2016 and 2017, respectfully.
How about the prescribers?
With so many pharmacies enabled for EPCS, and legislature allowing this process in all 50 states, it may be surprising to know that an average of 3.39% of prescribers were enabled to e-Prescribe controlled substances according to the 2015 Surescripts National Progress Report.
Lengthy and time-consuming software auditing and prescriber identity proofing processes are likely factors that have stalled prescriber adoption of EPCS, but for pharmacists, the initial setup is much easier. In addition, there have not been enough incentive for prescribers to adopt EPCS.
e-Prescribing was a requirement under the federal Meaningful Use Electronic Health Record (EHR) program, which incentivizes the use of EHRs through financial payments. However, e-Prescribing of controlled substances was specifically exempted from Meaningful Use Stages 1, 2, and 3. For these reasons, it isn’t surprising that in 2015 the state with the highest number of prescribers enabled was New York, as that was one of the only states with an e-Prescribing state mandate in effect at that time.
In 2015, New York had 26.6% of their prescribers enabled for EPCS, with Nebraska not far behind at 15%. Fast forward to December 1, 2016 and prescriber enablement has grown tremendously in some states, but remain dismally low in others. New York now has 71.5% of prescribers enabled, with no other state having even one-third of their prescribers enabled for EPCS. In fact, the average percentage for EPCS enabled prescribers remains even as of December 1, 2016, at only 8.4% despite all of the benefits of EPCS.
Why are these numbers so varied?
Electronic prescribing of controlled substances (EPCS) reduces fraud and keeps patients from getting multiple prescriptions for the same drug, so why are some states seeing major buy-in while other states are lagging? Much of this is impacted by states that have legislation in place to either require or reinforce the use of e-Prescribing, as outlined below.
Minnesota
Minnesota was the first state to implement an e-Prescribing mandate in 2008 in order to improve quality outcomes and efficiency in health care. The state mandate required prescribers, pharmacists, pharmacies, and pharmacy benefit managers (PBMs) to be up and running with e-Prescribing by January 1, 2011, however, only 13% of prescribers are actually enabled for EPCS as of late. Could this be because legislation doesn’t enforce its own law or penalize prescribers for not adhering to this legislature? Marty LaVenture, director of the Minnesota Office of Health IT and e-Health, seems to agree and notes, “policy levers could be used to encourage full adoption and use of e-Prescribing capabilities.”
New York
As you may already know, New York was the first state to require e-Prescribing of all prescriptions, both controlled and non-controlled, and the first to implement penalties for failing to adhere to this ruling. Penalties include, but are not limited to, loss of license, civil penalties, and/or criminal charges. With the highest rate of prescriber EPCS enablement, it’s evident that New York prescribers are taking this quite seriously.
Maine
Maine is the next state to implement an e-Prescribing regulation as of July 1, 2017 where all opioids prescriptions must be sent electronically. With only 0.6% of prescribers enabled for EPCS in the state according to the Surescripts report, and up to 2.9% as of the beginning of December 2016, it’s clear that Maine has a long way to go for all prescribers to be ready to follow this regulation.
In Summary
Although it’s legal in all 50 states, and there are many reasons EPCS is safer than on paper or another method, there is still a great discrepancy between EPCS enabled pharmacies and EPCS enabled prescribers due in part to the strict requirements put in place on the prescribers. While the statistics referenced here show that provider adoption of EPCS is still low in comparison to the pharmacy adoption we have seen, it’s important to remember that the e-Prescribing of non-controlled substances also took years to reach the level we now see today. It seems the only tried and true way for these numbers to rise quickly and meet the numbers we currently see for pharmacy enablement is to implement regulations and penalties for not adhering to this requirement as outlined in the above state mandates. All eyes are now on Maine to see how their journey goes.
Check out the maps below to see how your state measures up!
Author: Lindsey W.
Sources: American Pharmacists Association; USA Today; Surescripts 2015 National Progress Report; Surescripts EPCS; Minnesota Department of Health; Maine Medical Association; e-Prescribing Blog; CMS
About DoseSpot
DoseSpot is a Surescripts certified e-Prescribing platform specifically designed to integrate with electronic health record, electronic dental record, practice management, and telehealth software. DoseSpot is certified to e-Prescribe controlled substances and has provided simple, affordable and integratable e-Prescribing to more than 150 health care software companies since 2009. For more information, please visit www.DoseSpot.com.
Posted: October 6th, 2016 | Author: Shauna | Filed under: Controlled Substances, Digital Health, Telehealth | Tags: behavioral health, Care Coordination, Controlled Substances, DEA, Dental e-Prescribing, digital health, DoseSpot, e-Prescribing, e-Prescribing controlled substances, e-Prescribing Integration, e-Prescribing Software, EHR, EHR software, EPCS, Geriatric Care, Geriatrics, health IT, healthcare IT, Healthcare Software, healthIT, meaningful use, medication adherence, Opioid Epidemic, Opioids, Patient Engagement, technology, telehealth, telemedicine, trends, Value Based Care | No Comments »

It’s no surprise that technology should be considered a key player as we shift to value-based care. With smartphones, tablets and computers, health information is readily available for patients with a simple click of a button. Why should a consultation with a healthcare professional be any different?
Telehealth greatly increases the scope of the healthcare industry and is bound to open huge opportunities in increasing the quality of healthcare. The ultimate goal here, is to prevent hospital readmissions through better management of individuals with chronic conditions, while also reducing associated costs. By enabling remote patient monitoring and remote access to clinicians, market growth is inevitable as awareness and implementation of standards for reimbursement and adoptions of these care models expands.
While several reports claim that “technology gets in the way of the patient experience,†patients are in fact the ones demanding such access to care. This increase in patient demand for telehealth services has prompted many companies and healthcare organizations to think outside of the box and reevaluate the patient-centric model, while questioning what that care model really means to a patient.
Well, it’s simple. Patients want a customized, cost-effective and convenient healthcare experience to which telehealth can provide.
A recent report states that the global telehealth market was valued at $14.3 Billion in 2014 and is estimated to reach $36.3 Billion by 2020, growing at a CAGR of 14.30% from 2014 to 2020.
With these numbers in tow, we predict the most growth in three different segments:
Behavioral Health and Addiction
As mentioned in a previous post, telehealth has the ability to bridge the gaps in care of behavioral health patients and providers. Not only does it provide a convenient, more comfortable and less expensive medical consultation, but it broadens accessibility to patients whom may not have many options when seeking a behavioral health provider, especially in rural areas. Unfortunately, the lack of psychiatrists and addiction specialists across the nation, as well as the stigma often involved, are contributing to the mental health and addiction issues and creating barriers to appropriate care.
Patients will see their primary care physician and may not receive the exact treatment plan that they need; after all, primary care physicians do not specialize in behavioral health or addiction and often, these illnesses require a lot of time and patience to which the physician may not be able to accommodate. Telehealth will be able to connect patients in need with specialists regardless of their location who know how to treat these specific health issues.
This effective care model will not only lessen the hit on the nation’s bottom line as more and more individuals grapple with suicide, addiction, and other mental health issues, but also revolutionize the way people view the stigma involved and encourage patients to seek help as they are able to receive treatment from the comfort of their own home.
Geriatric Care
Geriatric patients stand to benefit tremendously as a digital health consumer. As mobility can be especially difficult for these patients, the ability to see a physician remotely removes one of the largest barriers to care. Furthermore, transporting patients of this age may potentially do more harm than good.
With telemedicine, providers can more quickly spot at-risk patients and provide interventions to avoid an otherwise unnecessary hospital admission. Similarly, nursing homes can partner with health systems to provide bedside care for their residents at a fraction of the price of an onsite physician.
These infrastructure synergies provide connectivity with electronic health records (EHRs) and create clear communication among hospitals, senior care facilities, referring physicians and patient families. They also provide the link to population based management databases and other health care analytic functions to measure value.
Surgery
Many surgical departments find telehealth to be a more convenient and cost-effective way for pre- and post- operative instructions for procedures of all magnitudes including wisdom teeth extraction, colonoscopies, stent placement and more.
With in-person visits and paper instructions, patients may misinterpret or even forget important information relative to their surgery. This includes what medications to stop taking and how to physically prepare for surgery, while providing a clear, direct line of answers for any questions a patient may have. With instructions digitally delivered prior to surgery, telehealth reduces patient no shows and saves valuable scheduled operating room time.
For post-op patients, providers can check the patient visually, ensuring that patients are following their treatment plans and making adjustments as needed. Through this continuous connection, providers are empowered to deliver the guidance that many patients need as they go through the healing process. These virtual check-ins ensure the patient is on the road to recovery, thus reducing readmission rates all without the patient ever having to leave their home.
Furthermore, telehealth can improve treatment and medication compliance, specifically with controlled substances, i.e. pain medication. Opioid addiction often begins at the hands of a prescriber and with the nation currently facing an opioid epidemic, marrying technology and follow-up appointments when prescribing these types of medications serves as the optimal solution for the safety of all involved.
Technology should no longer be viewed as a barrier to care, but rather embraced in order to improve the healthcare industry, including the improvement of interoperability as well as patient outcomes. Telehealth not only meets the ever increasing demands of patients, but it also assists in preventative care by creating greater access to such care, thus reducing down-the-road costs and burdensome associated with chronic disease. With many chronic diseases being completely preventable, the prevent vs. treat mantra should be sound in every healthcare professional’s mind, while realizing that telehealth is a seamless way of delivering healthcare for all involved.
There may currently be barriers in place regarding reimbursement from payers, but that’s sure to change as more and more payers jump on board for this new delivery model. After all, who’s to say telehealth won’t become the norm and be known as simply….health?
Sources:Â American Well; OpenPR; mHealth Intelligence; Healthcare IT News
About DoseSpot
DoseSpot is a Surescripts certified e-Prescribing platform specifically designed to integrate with electronic health record, electronic dental record, practice management and telehealth software. DoseSpot is certified to e-Prescribe controlled substances and has provided simple, affordable and integratable e-Prescribing solutions to healthcare IT companies since 2009. For more information, please visit www.DoseSpot.com.
Posted: March 9th, 2015 | Author: Lindsay | Filed under: Basics, In the News, Incentives, Public Policy, Uncategorized | Tags: CMS, DoseSpot, e-Prescribing Integration, EHR, healthcare IT, Healthcare Software, implementation, incentives, interoperability, meaningful use, MU3 | No Comments »
As the days of March begin to pick up, so do developments in the Healthcare IT arena. Washington insiders recently began speculating that the Centers for Medicare and Medicaid Services (CMS) will release Stage 3 meaningful-use (MU3) rules later this month. Per usual, ideas are already circulating as to what these rules will—and should—include.
According to the 2009 American Recovery and Reinvestment Act, the third stage of the incentive program will have a primary focus on data-sharing, or interoperability (a surefire MU3 “buzzwordâ€). While rules provide adequate guidelines for adoption, many healthcare professionals would like to see actionable results—such as Athenahealth’s Vice President of Government & Regulatory affairs, Dan Haley. In a recent article published in Modern Healthcare, Haley stated that the rules for MU3 should also require the “actual sharing of records rather than merely [setting] standards for how to accomplish interoperability…Providers should be able to see in one place a summary of a patient’s longitudinal health history…Without the need to [access] multiple systems.â€
In addition to MU3 implementation suggestions, many healthcare professionals have expressed interest in seeing new tech-savvy “bells and whistles.†Some are pushing for better “unique device identifier†support, which would allow public health officials to track specific devices through the vast healthcare system. Another purported new standard for technology could be the inclusion of “patient-generated health data†from devices including fitness monitors and health-tracking apps, which may help clinicians track the day-to-day lifestyles of patients in innovative ways. Stay tuned for the official release of MU3 requirements towards the end of this month!
SOURCE: Modern HealthcareÂ
About DoseSpotÂ
DoseSpot is a Surescripts certified e-Prescribing platform specifically designed to integrate with electronic health record, electronic dental record, practice management and telehealth software. DoseSpot is certified to e-Prescribe controlled substances and has provided simple, affordable and integratable e-Prescribing solutions to healthcare IT companies since 2009. For more information, please visit www.DoseSpot.com.
Posted: July 3rd, 2014 | Author: Jodi | Filed under: Basics, Controlled Substances, In the News, Newsletter | Tags: DoseSpot, e-Prescribing, e-Prescribing Integration, e-Prescribing Software, EHR, global, healthIT, meaningful use, trends, World Cup | No Comments »
The World Cup has us all thinking from a more global perspective.  Whether you call it soccer or football, the sport continues to gain popularity worldwide.  Also increasing prevalence across nations is e-Prescribing.  According to a recent market report by Transparency Market Research, the global e-Prescribing market is expected to reach $887 million by 2019, up from $250.2 million in 2013.  It’s not yet in the billions like the World Cup but it’s an impressive figure and speaks to the momentum health IT is gaining.
The report highlights that while Europe is the largest market for e-Prescribing, North America is currently the fastest growing e-Prescribing market in the world.  The remarkable growth is in large part due to the various government programs requiring e-Prescribing integration to improve care quality and reduce errors.  Government initiatives are also contributing to increased usage across Asia.  We forecast that industry adoption in North America will continue to increase as physicians want the capability to send prescriptions for controlled substances electronically (EPCS).
About DoseSpot
DoseSpot is a Surescripts™ certified e-Prescribing platform specifically designed to integrate with electronic health record, electronic dental record, practice management and telehealth software. DoseSpot has provided simple, affordable and integratable e-Prescribing solutions to healthcare IT companies since 2009. For more information, please visit www.DoseSpot.com.
Posted: July 2nd, 2014 | Author: Greg | Filed under: Basics, In the News, Standards, Telehealth, Venture funding | Tags: digital health, DoseSpot, e-Prescribing, e-Prescribing Integration, EHR, EHR software, Health Information Exchange, healthIT, meaningful use, rockhealth, surescripts, surescripts certification, trends, venture funding | No Comments »
RockHealth recently published their Digital Health Funding – Midyear Review and I’ve highlighted some key findings below:
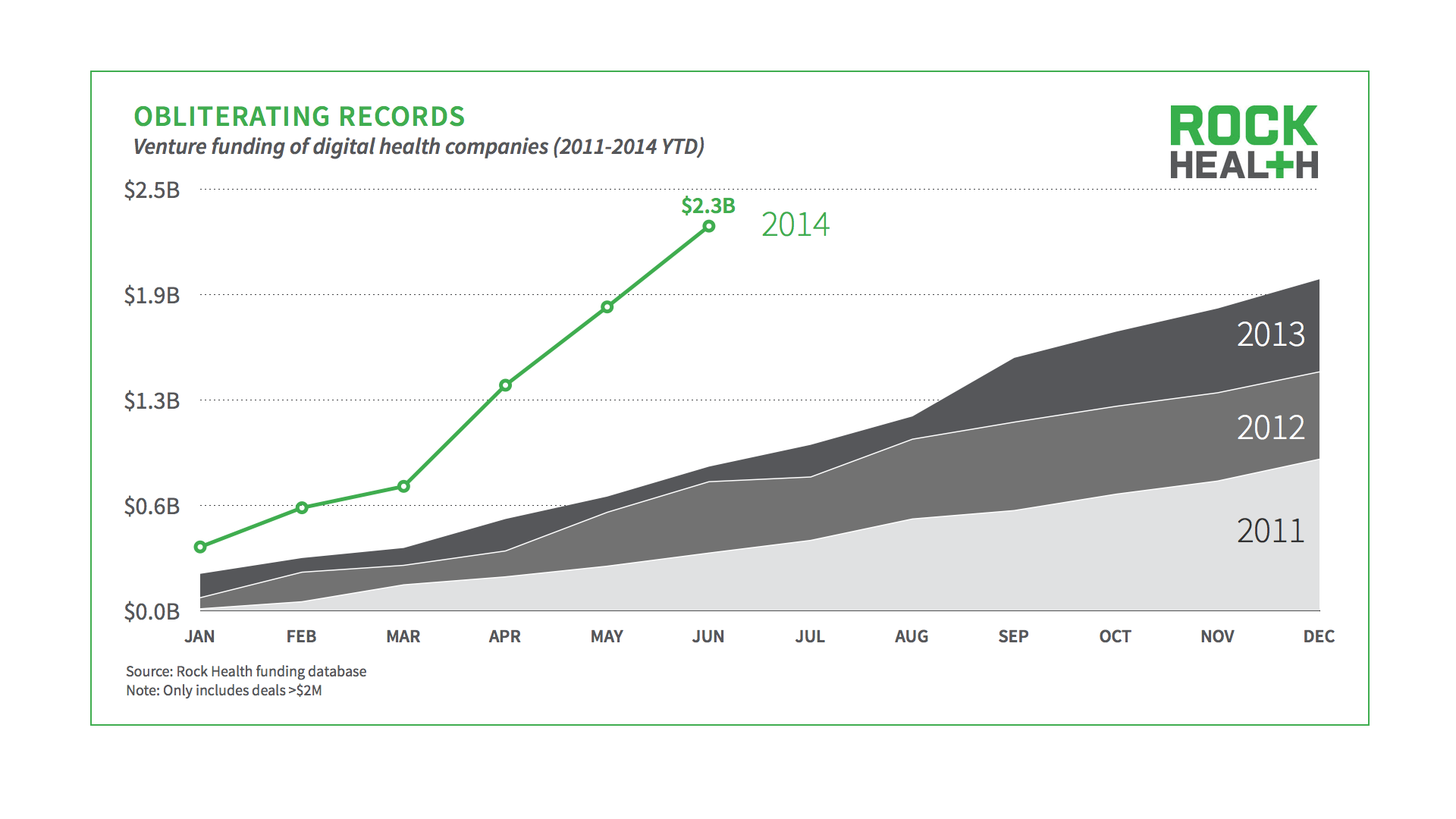
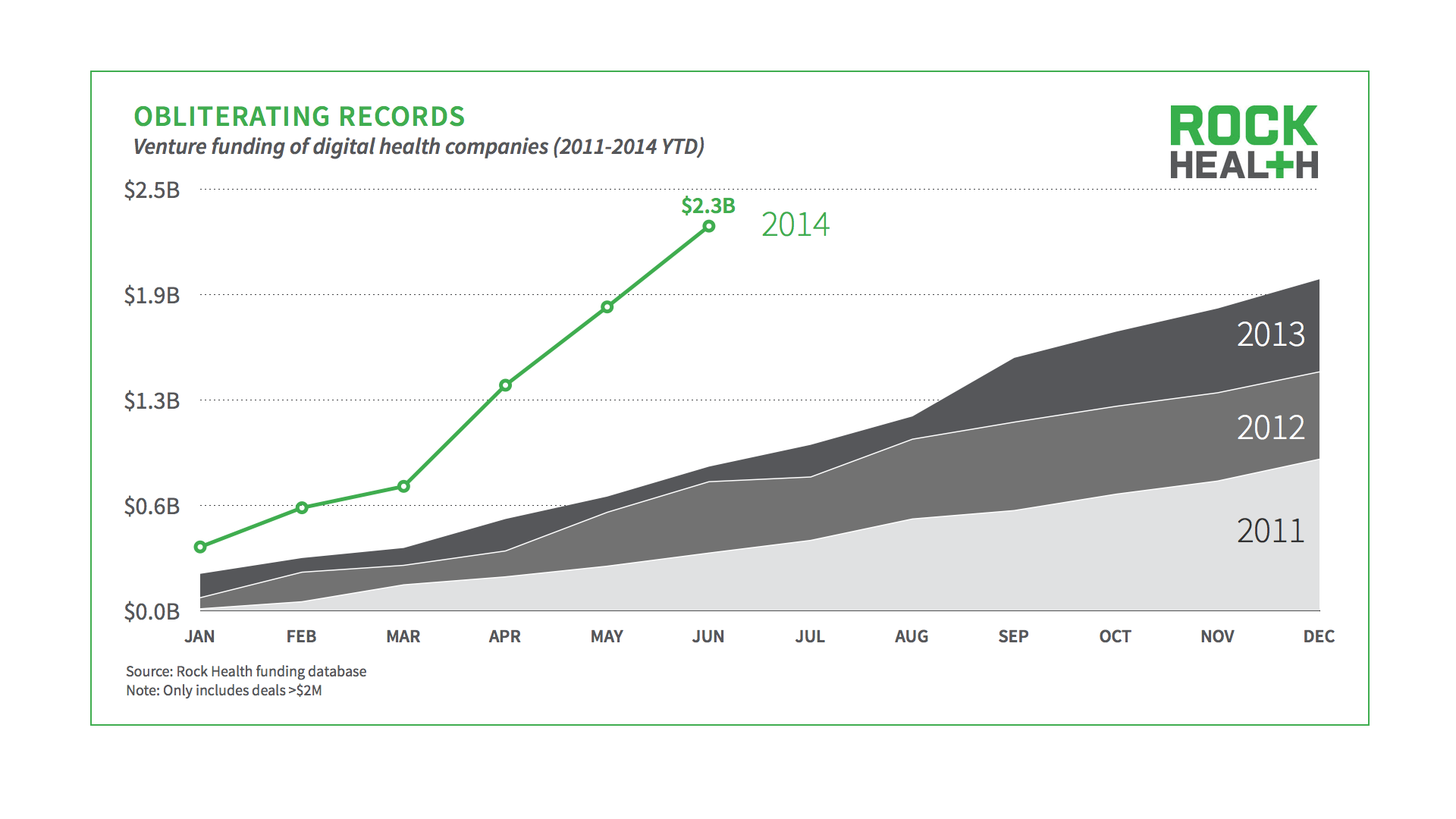
In 2013 digital health companies raised $2 billion in venture funding…first six months of 2014 digital health companies have already raised $2.3 billion.
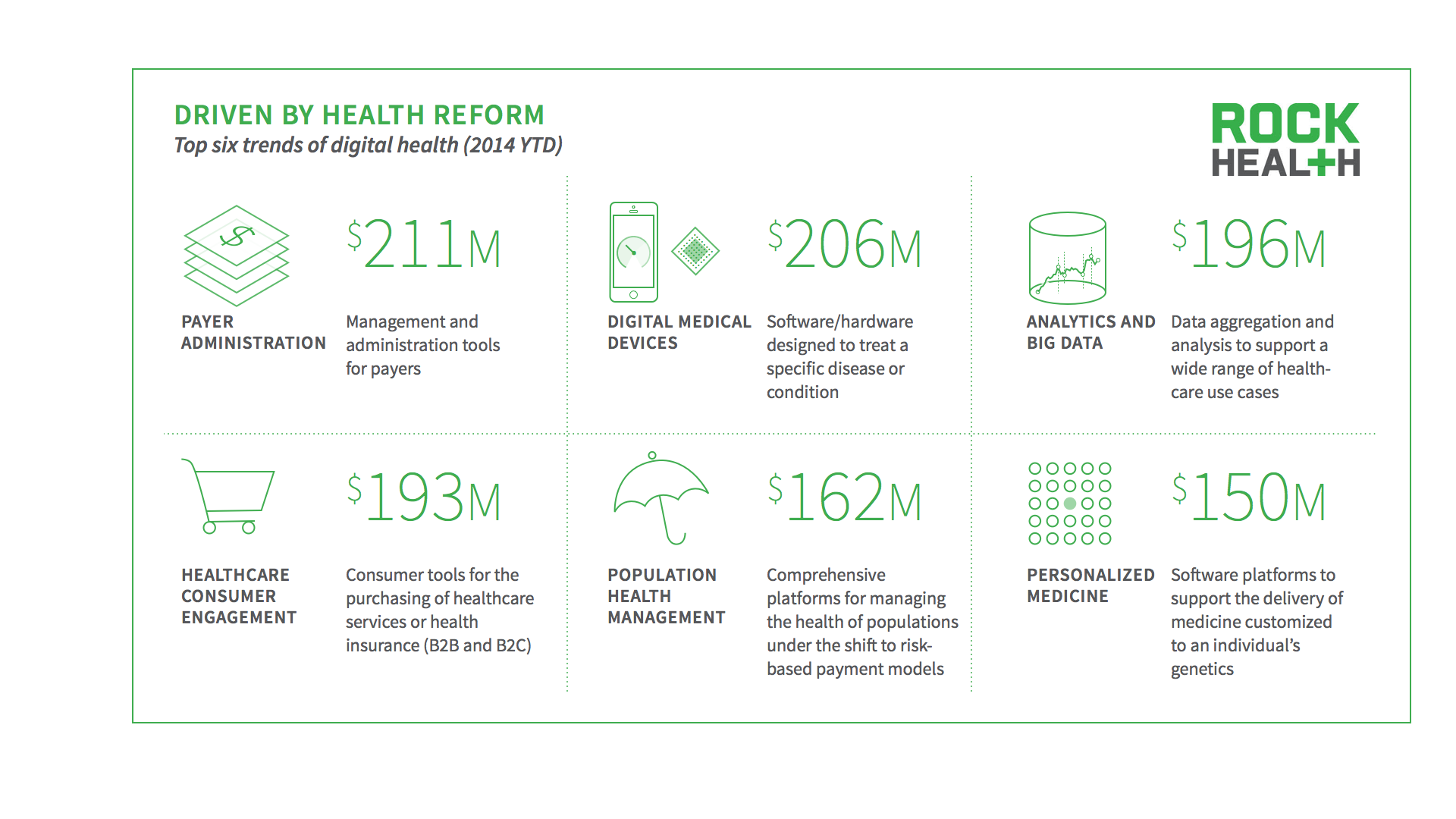
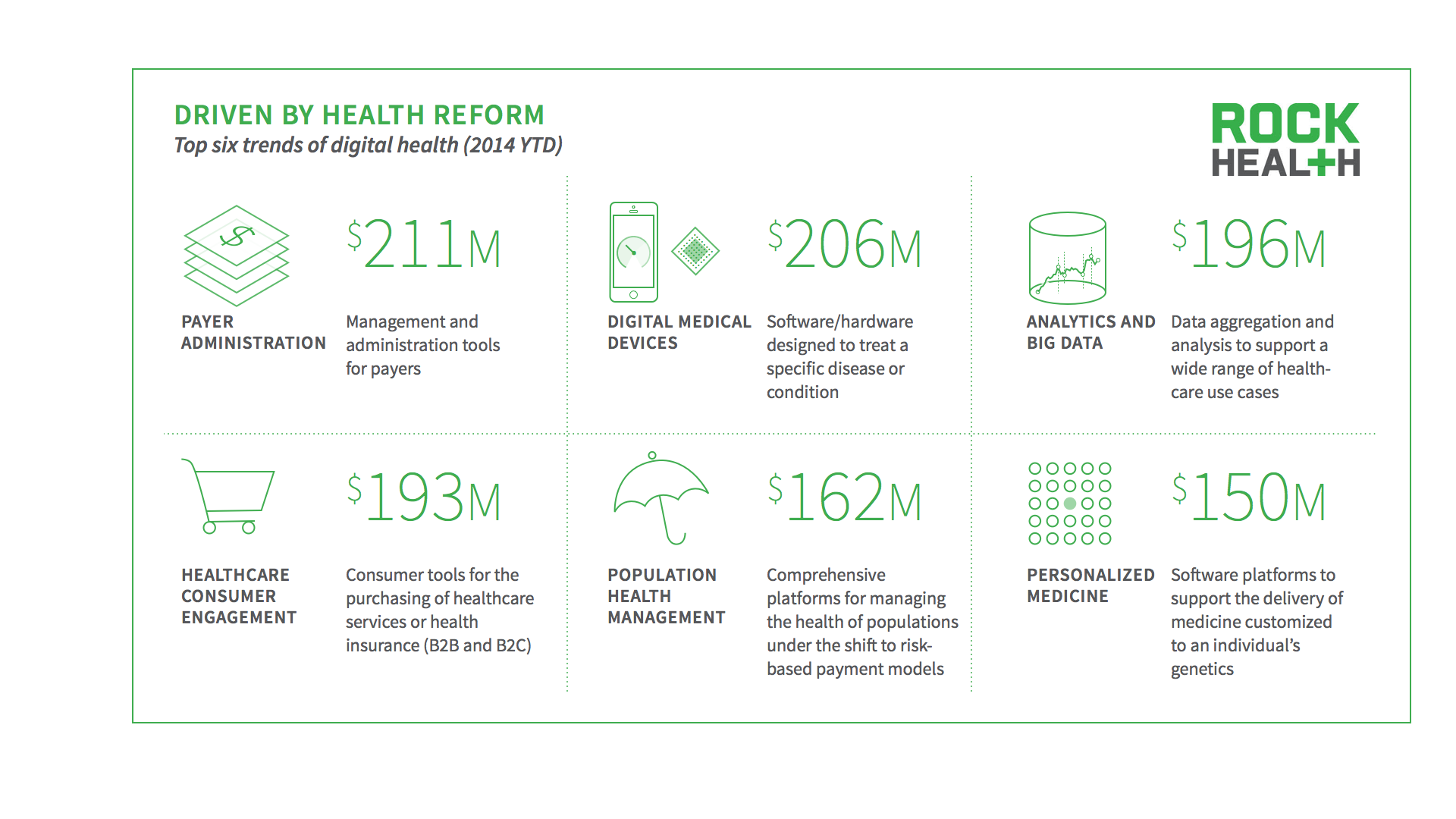
So where’s all the money going?
Here is the full report:
About DoseSpot
DoseSpot is a Surescripts™ certified e-Prescribing platform specifically designed to integrate with electronic health record, electronic dental record, practice management and telehealth software. DoseSpot has provided simple, affordable and integratable e-Prescribing solutions to healthcare IT companies since 2009. For more information, please visit www.DoseSpot.com.
Posted: June 25th, 2014 | Author: Greg | Filed under: Basics, In the News, Newsletter, Public Policy, Standards | Tags: #dosespotted, DoseSpot, e-Prescribing, e-Prescribing Integration, e-Prescribing Software, EHR, EHR software, healthIT, meaningful use, surescripts, surescripts certification | No Comments »
Surescripts recently published their annual National Progress Report highlighting advances in e-Prescribing throughout the United States. Without a doubt e-Prescribing is ‘here to stay’ and DoseSpot continues to be at the forefront of e-Prescribing integration services.
Below are a few key figures from the National Progress Report:
#1. More than 1.04 Billion e-Prescriptions were sent in 2013.

#2. 699 Million medication histories were delivered which often assist in limiting drug-drug interaction errors.

#3. Office-based physician adoption continues to grow and currently stands at 73%.

#4. 95% of pharmacies have adopted e-Prescribing.

About DoseSpot
DoseSpot is a Surescripts™ certified e-Prescribing platform specifically designed to integrate with electronic health record, electronic dental record, practice management and telehealth software. DoseSpot has provided simple, affordable and integratable e-Prescribing solutions to healthcare IT companies since 2009. For more information, please visit www.DoseSpot.com.
Posted: April 29th, 2014 | Author: Jodi | Filed under: Basics, In the News, Incentives, Newsletter, Public Policy, Standards | Tags: CMS, DoseSpot, e-Prescribing, e-Prescribing Software, EHR, EHR software, healthIT, meaningful use, MU, ONC, Stage 2 | No Comments »
Looking for tips to navigate MU stage 2 requirements?  View one tip on drug-drug and drug-allergy interaction checks below and visit http://www.dosespot.com/meaningful-use-tips to download all 5 certification tips!
Meaningful Use Stage 2:Â Tip #2Â –
§ 170.314(a)(2) Drug-drug, drug-allergy interaction checks
Objective:Â In addition to providing drug-drug and drug-allergy interaction checks, this criteria requires EHRs to adjust the level of interactions based on user roles (ie: administrator).
Tip:Â Provide an easy-to-use user interface so a user can quickly adjust the interactions. DoseSpot allows the user to turn on and off the drug-drug and drug-allergy interactions as well adjust the severity level display between minor, moderate and major interactions.
Click here for more blog posts at ePrescribing.org on Meaningful Use.
Posted: March 11th, 2014 | Author: Greg | Filed under: Basics, In the News, Incentives, Newsletter, Public Policy, Standards | Tags: DoseSpot, e-Prescribing, e-Prescribing Integration, e-Prescribing Software, EHR, healthIT, meaningful use, mental health, ONC, surescripts certification | No Comments »

About Bear River Mental Health:
Bear River Mental Health (BRMH) provides comprehensive mental health services to more than 3,000 patients annually at their eight locations across Utah. Delivering mental health services according to the best practice guidelines with respect to appropriate medical necessity for more than 35 years, BRMH offers an array of services including:
• Assessments
• Behavior Management
• Crisis Management
• Medication Management
• Peer Support
• Psychological Testing
• Psychosocial Rehabilitation
• Psychotherapy
• Residential Services
• Respite Care
• Skills Development
e-Prescribing Integration:
“DoseSpot support is second to none†exclaims Thad Hunsaker, BRMH. All eight of the BRMH offices use DoseSpot, with physicians accessing the e-Prescribing solution from multiple locations. Thad explains, “Geographic location hasn’t added any difficulty where the service is provided online.†As a mental health organization, BRMH uses DoseSpot for more than just e-Prescribing. “Patient medication management has long been an integral part of our treatment. DoseSpot helps us manage this process online†adds Thad. DoseSpot equips physicians with the capabilities to build a patient’s medication profile and then automatically review any drug-drug and drug-allergy interactions.
For the rest of this Case Study please visit http://www.dosespot.com/bear-river-mental-health.
Posted: March 3rd, 2014 | Author: Jodi | Filed under: Basics, Incentives, Newsletter | Tags: CureCompanion, DoseSpot, e-Prescribing, e-Prescribing Software, EHR, EHR software, healthIT, meaningful use, OpenEMR | No Comments »
OpenEMR is an electronic health record (EHR) and practice management application that can be downloaded with the click of a button. OpenEMR has a longstanding reputation as an open-source software (OSS) solution, after first being established 10+ years ago. It is ONC Complete Ambulatory EHR certified and qualifies physicians using the software for meaningful use incentive payments. EHR companies like CureCompanion have successfully integrated a mobile friendly interface layer on top of OpenEMR, running on a secure cloud.
OpenEMR includes a wide-range of features including:
• Patient Demographics
• Patient Scheduling
• Electronic Medical Records
• Medical Billing
• Clinical Decision Rules
• Patient Portal
• Reports
• Multilanguage Support
• Security
• Free Support
What is the only thing missing from OpenEMR? The answer is e-Prescribing. DoseSpot e-Prescribing can and has been integrated into an OpenEMR solution seamlessly and in just a short amount of time. e-Prescribing integration expands on the long list of features to include the routing of new and refill prescriptions electronically, drug-drug and drug-allergy interaction checking, ability to view a patient’s medication history and check their insurance eligibility and formulary information.
To learn more about DoseSpot e-Prescribing, visit www.DoseSpot.com.
Posted: February 6th, 2014 | Author: Greg | Filed under: Basics, In the News, Incentives, Newsletter, Standards | Tags: DoseSpot, e-Prescribing, e-Prescribing Integration, e-Prescribing Software, EHR, EHR software, healthIT, ipad, iPad e-Prescribing, meaningful use, mobile, mobile e-Prescribing, mobile health it, ONC, surescripts, surescripts certification | No Comments »

Case Study:
One Touch EMR is designed to be simple and instinctive, allowing physicians to chart as fast as possible on their iPads and desktop computers. What makes their system unique is it was designed and developed by Dr. Robert Abbate, a physician who understands how physicians think and knows what is needed to provide an effective EMR solution that removes complexities rather than adding obstacles. Dr. Abbate designed One Touch EMR to replicate the medical school workflow students are trained in, making the solution more intuitive to physicians with the perks of being affordable and mobile. One Touch EMR is Stage 1 Meaningful Use certified and is used by more than 400 physicians across the United States.
e-Prescribing Integration:
During the planning and development stages of the One Touch EMR app, Dr. Abbate searched for an e-Prescribing platform that would seamlessly connect with his sleek and intuitive user interface. After thoroughly reviewing his options, Dr. Abbate selected DoseSpot because of its quick integration and easy to use user interface.
For the rest of this Case Study please visit www.DoseSpot.com/onetouchemr-case-study .


 Follow
Follow