Posted: March 2nd, 2017 | Author: DoseSpot | Filed under: In the News, Public Policy | Tags: e-Prescribing, e-Prescribing controlled substances, Electronic Prescription, EPCS, health IT, healthcare IT, Healthcare Software, Maine State Mandate, Minnesota State Mandate, Opioid Epidemic, State e Prescribing Law, State e Prescribing Mandate, State Electronic Prescription Law, State Electronic Prescription Mandate, State Mandates, State Opioid Law | No Comments »
It’s no secret that e-Prescribing has its benefits. Many professionals agree that eRx greatly improves patient safety and reduces overall health care costs by lowering potential medication errors. Additionally, the ability to electronically prescribe controlled substances (also known as EPCS) greatly reduces fraud while preventing patients from being able to “doctor shopâ€, or receive multiple prescriptions for the same drug via different prescribers.
According to Paul Uhrig, Chief Legal Officer for Surescripts, between 3-9% of all opioid abusers use or have used forged prescriptions. With e-Prescribing, the ability to forge prescriptions is completely taken off the table. On top of that, with the addition of Prescription Drug Monitoring Programs (PDMPs) now implemented in all 50 states, prescribers are able to see all pertinent data that has been pulled from the patient’s electronic health record (EHR). This inevitably helps them make more knowledgeable and appropriate choices when prescribing scheduled medications.
With so many known benefits of e-Prescribing, and also because of the nationwide opioid epidemic, many states are getting on board the mandate train, which requires that by law, all prescribers must submit prescriptions electronically. There are currently 3 states which have this e-Prescribing mandate: New York, Maine, and Minnesota and many more that already have legislation in the works for an e-Prescribing mandate.
Taking the First Step: Minnesota Mandate
Minnesota was the first state to create an e-Prescribing mandate, which was intended to push all prescribers to establish and maintain an electronic prescription program that complied with state standards (listed here), effective January 1, 2011. According to the Minnesota Department of Health (MDH), Minnesota measures the status of e-Prescribing in three ways: total transactions, enabled pharmacies, and prescriber utilization. They’ve provided the following chart to demonstrate the increase in e-Prescribing transactions since 2008:

We can see that there was a pretty steep jump in 2011, which is when the mandate went into effect. However, the climb from 2011-2013 was slow yet steady.
Reinforcement of the Mandate, or Lack Thereof
The Minnesota Department of Health reiterates that there is currently no enforcement mechanism for not complying with the state’s e-Prescribing mandate. MDH does stress the benefits of e-Prescribing to providers as well as threaten with the possible implications of non-compliance from a patient/healthcare perspective. When the mandate was first released, it was implied that there would most likely be future establishment of enforcement methods. However, as of today, there is still no means of forcing providers to comply with the mandate.
Because there are no negative repercussions to providers who do not comply, there are many that choose to still utilize paper prescriptions, especially when it comes to sending controlled substances. According to Surescripts, only 3.5% of doctors in Minnesota were using EPCS in 2016. Additionally, the Minnesota Department of Health showed that drug overdose deaths increased 11%, reporting 516 deaths in 2014 to 572 deaths in 2015. These statistics could very well be unrelated to each other, but it still goes to show that that there is work to be done in Minnesota in regards to the opioid epidemic and electronic prescribing.
Some Considerations
Even though there is proof that it has its benefits, the challenges that come with implementing e-Prescribing can’t be ignored. Understandably, and rightfully so, prescribers have long expressed that their main focus is on their patients and they generally don’t enjoy being dictated by the government if it means being intrusive in helping their patients. This is especially true when it involves new systems that require onboarding and training time, but it can also be an even bigger challenge for prescribers to find the funds to support the implementation of an e-Prescribing system.
With these two large considerations in mind, it’s important that future states not only allow healthcare software companies and associated practices ample time to get their e-Prescribing systems up and running, but also offer some form of incentive or enforcement mechanism to keep prescribers in compliance. However, it’s even more important to remind prescribers that the perceived difficulty during the transition time in the beginning is minimal in comparison to how many benefits will transpire in the future. It’s all about taking that first step.
Author: Shannon K.
Sources:Â Minnesota Department of Health; Minnesota Department of Health Fact Sheet; MN e-Prescribing Guidance; Decision Resources Group; USA Today; Managed Care Magazine
About DoseSpot
DoseSpot is a Surescripts certified e-Prescribing platform specifically designed to integrate with electronic health record, electronic dental record, practice management and telehealth software. DoseSpot is certified to e-Prescribe controlled substances and has provided simple, affordable and integratable e-Prescribing solutions to healthcare IT companies since 2009. For more information, please visit www.DoseSpot.com.
Posted: February 28th, 2017 | Author: Jodi | Filed under: In the News, Public Policy | Tags: Connecticut e-Prescribing Bill, Connecticut Opioid Bill, Connecticut Opioid Law, Connecticut Opioid Legislation, Connecticut Opioid Proposal, e-Prescribing, electronic prescribing, Electronic Prescription Law, Electronic Prescriptions, EPCS, Maine e-Prescribing Mandate, Maine Mandate, Maine Opioid Law, Maine Opioid Prescribing Mandate, Maine Opioid Prescriptions, Mandatory e-Prescribing, Mandatory Electronic Prescribing, Opioid Abuse, Opioid Crisis, Opioid Drugs, Opioid Epidemic, Pennsylvania e-Prescribing Bill, Pennsylvania Opioid Bill, Pennsylvania Opioid Law, Pennsylvania Opioid Legislation, Pennsylvania Opioid Prescriptions, State e Prescribing Law, State e Prescribing Mandate, State Opioid Law, State Opioid Mandates, Virginia e-Prescribing Law, Virginia e-Prescribing Mandate, Virginia Opioid Bill, Virginia Opioid Law, Virginia Opioid Legislation, Virginia Opioid Mandate, Virginia State Mandate | No Comments »

New York will soon be celebrating their one year e-Prescribing mandate anniversary at the end of March and on the heels of this inaugural, impactful mandate, it’s exciting to see other states hopping on the e-Prescribing bandwagon. Not only did Maine announce its own e-Prescribing legislation that’s effective in just four months, but since the start of 2017, three additional states have introduced similar mandates. One common denominator most prevalent to note, however, is the overwhelming commitment by each state to combat the opioid crisis in order to decrease overdose death rates and improve patient safety overall.
Let’s review the three states that have recently proposed e-Prescribing legislation.
Pennsylvania
Pennsylvania experienced an astounding 3,264 opioid overdose deaths in 2015, a 20.1% increase from 2014. With the rising, devastating numbers in tow, Pennsylvania has decided to take further action and follow suit with New York and Maine.
On February 6, 2017, Pennsylvania State Senator Richard Alloway and Pennsylvania State Representative Tedd Nesbit announced the introduction of legislation that will require all opioid prescriptions such as OxyContin®, Percocet®, and Norco® to be e-Prescribed in Pennsylvania. The proposed bill will not only require controlled substances to be sent electronically, but will also enforce Schedule II medications not to be refilled by the pharmacy. For Schedules III and IV prescriptions, the bill requires that such prescriptions, “shall not be filled or refilled more than six months after the date thereof or be refilled more than five times after the date of the prescription unless renewed by the practitioner.â€
The state is committed to a fast turnaround on implementing this legislation and as a result, especially for the protection of patients, the General Assembly is being urged to pass this vital legislation before June 30, 2017.
Connecticut
Yet another state devastated by the increasing drug overdose deaths from opioids, Connecticut Governor Dannel Malloy recently announced an increase in state funding to address opioid addiction and also introduced a series of legislative proposals, including one that will require all opioid prescriptions to be electronically prescribed. Governor Malloy not only highlighted the reduction in fraud that e-Prescribing can accomplish relative to curbing drug diversion, but also specifically noted the benefits of being able to track prescription data as a means to document both prescriber and patient information for electronic transactions.
“A pad of paper doesn’t come from a particular site. It is hard to trace,†Malloy said. “If you do it electronically, you can instantaneously trace, and it’s easier for us to document who is getting the drug, and who is prescribing the drug.â€
As part of Governor Malloy’s proposal, a bill that outlines giving patients the ability to include a form in their medical file that indicates that they do not want opioid treatment has also been included. With value based care underway, this serves as another way to encourage patients to make their own health care and treatment decisions for what they deem works best for them.
Like Pennsylvania, the protection of patients across Connecticut is of utmost importance to the state, therefore Governor Malloy is pushing for this imperative legislation to be effective as of January 1, 2018.
Virginia
In Virginia, it has been estimated that 1,000 people died from overdose in 2016, a 33% increase from the prior year. Moving quickly, the General Assembly of Virginia unanimously approved legislature on January 26, 2017 requiring any prescription containing an opiate to be issued as an electronic prescription and will also prohibit any pharmacist from dispensing a controlled substance that contains an opiate unless the prescription is issued electronically.
On February 23rd, Virginia Governor Terry McAuliffe signed five bills to address the opioid epidemic, including the mandate for all opioid prescriptions to be prescribed electronically by July 1, 2020. It will also create a working group to study how best to implement this change.
What’s unique about this legislature, however, is that it all began with a practicing dentist who happens to be a state delegate for Virginia.
“We have all seen the tragic headlines that highlight the devastating impact that opioid addiction has had – and continues to have – on families and communities throughout the Commonwealth and the Nation,†said Delegate Todd Pillion. “This is an issue that I see not only as a legislator, but as a prescriber myself.â€
As such, Delegate Pillion decided to utilize his profound, and heartfelt, voice to address the opioid epidemic that is sweeping our nation at alarming rates. Having personal experience under his belt, he was responsible for the original proposed e-Prescribing mandate in Virginia.
Where do other states stand?
With 3 states proposing legislature in the first 60 days of 2017, we anticipate more states to follow. As many individuals involved in the aforementioned state legislations have mentioned, it just makes plain sense to prescribe the most addictive, but necessary, medication through e-Prescribing. It is finally, and rightfully, being viewed as an optimal tool to overcome this drug crisis.
Electronically prescribing opioids will not only decrease drug overdose deaths and increase patient safety, but it will also:
- Combat the rising issue of prescription fraud within a dental practice, including misuse of a dentist’s DEA number, forged signatures, and stolen prescription pads by patients or an Insider Threat.
- Allow a prescriber to query a patient’s medication history at point of care in order to determine if they are “doctor shoppingâ€, or visiting multiple prescribers strictly to receive opioid prescriptions.
- Add to patient convenience by reducing wait times in pharmacies.
- Increase patient medication pick-up adherence. Between 28% and 31% of all paper prescriptions either never make it to the pharmacy or are not picked up at all.
Stay tuned for more states that will undoubtedly be proposing similar legislature in order to work together toward a common goal for the safety of patients overall.
Sources: Virginia Gazette; Bearing Drift; Centers for Disease Control and Prevention; CBS Local; WNPOR
About DoseSpot
DoseSpot is a Surescripts certified e-Prescribing platform specifically designed to integrate with electronic health record, electronic dental record, practice management and telehealth software. DoseSpot is certified to e-Prescribe controlled substances and has provided simple, affordable and integratable e-Prescribing solutions to healthcare IT companies since 2009. For more information, please visit www.DoseSpot.com.
Posted: February 8th, 2017 | Author: DoseSpot | Filed under: Basics, Controlled Substances, Public Policy | Tags: Controlled Substances, Government Opioid Road Map, Government Road Map, Maine e-Prescribing Law, Maine e-Prescribing Legislation, Maine e-Prescribing Mandate, Maine Mandate, Mandatory e-Prescribing, Mandatory Electronic Prescribing, National Governors Association, NGA, Opioid Abuse, Opioid Crisis, Opioid Epidemic, Opioid Overdose, Opioid Road Map, Opioids, PDMP, PDMP State Mandate, PMP, Prescription Drug Monitoring Program, Prescription Monitoring Program, Prescription Opioids, Schedule II Medications, State Mandate | No Comments »

The opioid crisis has taken our nation by storm, claiming an average of 78 victims a day, all of whom lost a vicious battle with opioid addiction. According to the National Governors Association, the current epidemic is being fueled by inappropriate opioid prescribing, as 4 out of 5 heroin users reported misusing prescription opioids before switching to heroin. Now, governors across the United States are taking action against the epidemic with a range of public health and safety strategies that address everything from prevention to treatment to recovery. In order to successfully attack the opioid crisis head on, they’ve decided to create an Opioid Road Map which will act as a tool to outline these strategies for states nationwide.
A Road Map Was Born
The Road Map was developed by the National Governors Association (NGA) to help states respond to the growing crisis of opioid abuse and overdose, as well as strengthen law enforcement efforts and abilities to address illegal activity. The individual state can either follow the road map step-by-step or they can pick and choose which pieces to utilize based on their needs.
The Opioid Road Map is a three-part process as outlined by the NGA:

Step 1 – Assess the Situation
Step 2 – Develop and Select Policies
Step 3 – Finalize Policies, Implement, and Evaluate Results
To develop the Road Map, the NGA worked with 13 states between 2012 and 2015 to create effective statewide programs to battle the opioid epidemic. Input was received from multiple stakeholders including pain specialists, law enforcement officials, health care payers, substance use disorder treatment professionals, and more. Numerous resources were shared in order to build this Road Map and having the ability to optimize and utilize the data collected from state Prescription Drug Monitoring Programs (PDMPs) was key to the Road Map’s creation.
The Role of PDMPs
The PDMPs of individual states is a database that contains controlled substance prescribing and dispensing data submitted by pharmacies and prescribers. This information is used to monitor and analyze all prescribing activity for use in abuse prevention, research and law enforcement. In regards to the Opioid Road Map specifically, the NGA is encouraging states to use their PDMPs as a tool for prescribers to gather real-time information on prescription opioids, and to analyze trends and outcomes associated with policies and programs.
According to the NGA, in order to maximize the use and effectiveness of state PDMPs, the following should be required:
- Prescribers should be querying PDMPs before prescribing Schedule II, III, IV controlled substances
- Pharmacists must report to the state’s PDMP within 24 hours of dispensing
- PDMP data must be used to provide proactive analyses and reporting to professional licensing boards and law enforcement
- PDMPs must be easy to use and PDMP data should be integrated into the Electronic Health Record (EHR)
- PDMPs should be interoperable with other states
Since these Prescription Drug Monitoring Programs already exist within forty nine states, it would be beneficial to utilize this data not only for preventing occurrences such as “doctor shopping†(people seeking multiple pain prescriptions from multiple prescribers) and identifying at risk patients, but also for achieving goals put forth by the Road Map in relation to research, law enforcement, and policy reform.
Road Map Expectations
By utilizing the Road Map, states will find background information on the current issue of opioid abuse and which factors are involved with prescription opioid misuse and addiction. They will also have access to the different steps outlined which act as a how-to guide for assessing the situation, selecting policies, and evaluating initiatives. Another item of value they could get from using the road map is a summary of evidence-based health care and public safety strategies to reduce opioid abuse.
By utilizing the Road Map, states will be able to work together to not only brainstorm about how to prevent and respond to the opioid epidemic, but more importantly, they will be able to put a plan into action which will achieve those defined objectives, with the ultimate goal of saving more lives in the process.
Author: Shannon K.
Sources: National Governors Association; NGA Road Map Outline; GCN Magazine
About DoseSpot
DoseSpot is a Surescripts certified e-Prescribing platform specifically designed to integrate with electronic health record, electronic dental record, practice management and telehealth software. DoseSpot is certified to e-Prescribe controlled substances and has provided simple, affordable and integratable e-Prescribing solutions to healthcare IT companies since 2009. For more information, please visit www.DoseSpot.com.
Posted: February 8th, 2017 | Author: DoseSpot | Filed under: Basics, Controlled Substances, Public Policy | Tags: Addiction, Addiction Treatment, American Medical Association, CDC, Controlled Substances, DEA, Drug Diversion, e-Prescribing controlled substances, e-Prescribing State Law, EPCS, Maine State Mandate, Mandatory e-Prescribing, Mandatory Electronic Prescribing, PDMP, PDMP State Law, PDMPs, PMP, PMPs, Prescription Drug Abuse, Prescription Drug Diversion, Prescription Drug Monitoring Program, Prescription Drug Monitoring Programs, Prescription Monitoring Program, Prescription Monitoring Programs, State Law, State Mandate | No Comments »

Prescription Drug Monitoring Programs (PDMPs) are state-run electronic databases that are used to track the prescribing and dispensing of controlled prescription drugs with the intent of helping to detect suspected abuse or diversion. These electronic databases provide important information regarding a patient’s controlled substance history that can be accessed by authorized individuals or agencies including law enforcement, medical examiners, addiction treatment programs, public and private payers, pharmacies, healthcare providers, and more.
All states except Missouri, the District of Columbia, and Guam have enacted PDMP legislation that mandate healthcare providers to record, consult and monitor prescribing data. Since the widespread implementation of PDMPs and corresponding legislations, there have been stories and statistics that seem to indicate success, however, there has also been feedback that indicates some major troubles with these databases and their use.
With PDMPs being utilized all over the country, should we expect a major turn-around in the prescription opioid crisis that is sweeping the nation? Are these databases in fact doing the job that they are intended to do? Or, are there major issues that are preventing their success? Let’s explore together.
The Benefits of PDMPs
PDMPs are considered to be the most promising state-level interventions to improve opioid prescribing, inform clinical practice, and protect patients at risk. They are intended to not only medically benefit patient care, but also to serve as a tool for law enforcement and other agencies concerned with opioid-related threats to the public health. This is because the information entered in to a PDMP can help prescribers and pharmacists identify patients at high-risk who would benefit from early interventions.
Further evaluations of PDMPs have demonstrated changes in prescribing behaviors, the use of multiple providers by patients, and decreased substance abuse treatment admissions. From a public health standpoint, PDMPs can be used by state health departments to better understand the current opioid addiction epidemic to better create new intervention methods.
As an example, in 2010, Florida established a PDMP and prevented health care providers from dispensing prescription opioid pain relievers directly from their office. That same year, there was a 50% decrease in oxycodone overdose deaths in the state. This change is thought to represent the first documented, substantial decline in drug overdose mortality in any state during the previous ten years.
Likewise, in 2012, prescribers in New York and Tennessee were required to check the state’s PDMP before prescribing opioids and the following year, New York saw a 75% drop in patients “doctor shopping†and Tennessee saw a 36% drop.
The Unfortunate Reality of PDMPs
Although PDMPs have significant potential to improve public health and patient outcomes, they do have the following shortcomings:
1. Under-Utilization
The inconsistent use, or under-utilization, of PDMPs is considered to be the biggest issue plaguing the database, as a PDMP is most useful when queried before prescribing and most maximized where usage is state mandated. A recent survey found that with physicians prescribing in a state without a PDMP mandate, only 22% were aware of their state’s PDMP, and only 53% had actually used it. These facts clearly indicate that state legislation is a critical success factor for the effectiveness of PDMPs to save patient lives.
2. Lack of Accessibility
Another issue with PDMPs is the ease of use and access, or lack thereof. States vary widely in which user categories are permitted to request and receive prescription history reports and under what conditions. Research suggests that usage may improve if states were to allow providers to appoint non-prescribing staff members to access the database on their behalf.
Furthermore, not all PDMPs share information across state lines. This can lead to important information being missed and can allow at-risk patients to receive more prescriptions for controlled substances than intended. However, more states are realizing the importance of sharing data across state lines and have recently become a part of PMP InterConnect.
3. Varying Times of Information Entry
Another matter of concern with PDMPs is varying times of information entry. When a controlled substance is dispensed to a patient, the prescription and patient information is entered by the pharmacy to the state PDMP. However, this information is entered at varying intervals – hourly, daily, or even monthly. If there is a long interval between dispense and submission times into the state PDMP, users will not have the most up-to-date information on a patient’s most recent prescriptions, thereby eliminating the maximum benefit of a PDMP. Currently, Oklahoma is the only state that collects data in real time, whereas, most states allow up to a week or longer for data submission.
4. Patient Adoption
Many prescribers attribute their worry about a patient’s reaction when checking the PDMP as a major disadvantage. In a recent survey, providers reported a variety of issues that arose when they reviewed the PDMP:
- 88% of patients reacted with anger or denial when questioned
- 73% of clinicians said that those angered patients sometimes did not return
- 22% of clinicians reported that the confronted patients had never asked for help with drug addiction or dependence problems
These clinicians also indicated that the unveiling of this information was not only upsetting to patients, and damaging to practitioner-patient relationships, but was also found to be inaccurate at times.
Additional concerns include added costs of more frequent office visits if prescribers become more cautious about writing prescriptions with refills, feelings of embarrassment when questioned about substance abuse, and patients turning to the illicit drug market if they are refused a controlled substance prescription.
Although the American Medical Association and American Society of Addiction Medicine stress the need to treat PDMP data just as well, if not better, than any other medical record, patients are becoming more vocal in their discomfort with PDMPs, claiming they make them feel that a medical consultation is no longer private.
5. Reluctant Prescribers
Like their patients, prescribers also show growing concern that they will be judged based on PDMP data. While most prescribers are assumed to support interventions to prevent fraudulent prescribing, high profile criminal prosecutions of prescribing large amounts of opioids can make prescribers reluctant to prescribe controlled substances in general for fear of legal retribution, also known as the “chilling effectâ€.
There is also greater perceived legal risk for prescribing or dispensing too much pain medication than for prescribing or dispensing too little pain medication. Because many practicing physicians have little if any formal training that would enable them to identify drug diversion, there is fear that PDMPs may wrongfully suspect and categorize some conscientious and caring physicians as fraudulent prescribers when they are actually prescribing in good faith, but lack training.
What Does This All Mean?
In this era of information technology, PDMPs are likely here to stay. While there are the aforementioned pitfalls of PDMPs, it is important to remember that there are still benefits to PDMPs in the public health sector, law enforcement, and of course, healthcare systems. What may be most helpful is to realize what changes could be made to make the PDMP process an ideal one.
From the standpoint of many prescribers, an ideal PDMP would:
- Alert its users to signs of illegal drug use
- Be easy to access
- Provide real time updates
- Be mandatory
- Have interstates accessibility
Perhaps over time if these changes were to be made, we would see more consistent use of PDMPs, especially as a tool to help overcome the opioid epidemic. A clear standard of practice against which providers’ care would be judged could also further advance the utilization of PDMPs in each state. Lastly, adequate training on addiction and pain management, along with a careful review of who should access a PDMP, could also attribute to better utilization and help accelerate the acceptance of each states’ prescription drug monitoring programs.
Author: Lindsey W.
Sources: Centers for Disease Control and Prevention; Lynn Webster MD; PDMP Assist;Â Wolters Kluwer; Shatterproof; National Center for Biotechnology Information
About DoseSpot
DoseSpot is a Surescripts certified e-Prescribing platform specifically designed to integrate with electronic health record, electronic dental record, practice management and telehealth software. DoseSpot is certified to e-Prescribe controlled substances and has provided simple, affordable and integratable e-Prescribing solutions to healthcare IT companies since 2009. For more information, please visit www.DoseSpot.com.
Posted: January 30th, 2017 | Author: DoseSpot | Filed under: Basics, Public Policy | Tags: e-Prescribing, e-Prescribing Platform, e-Prescribing Registration, e-Prescribing Software, e-Prescribing Solution, e-Prescribing State Mandates, New York e-Prescribing Mandate, New York e-Prescribing Registration, New York e-Prescribing Renewal, New York e-Prescribing Vendor Registration, New York e-Prescribing Vendor Renewal, New York Mandate, New York State Dental Association, New York State Department of Health, New York State Mandate, Registration for Official Prescriptions and e-Prescribing Systems, ROPES, State Mandates | No Comments »

If you are a prescriber in the state of New York, you probably know by now that electronic prescribing (e-Prescribing) of both controlled and non-controlled substances has been mandatory since March 27, 2016. As part of this mandate, all prescribers who will be sending controlled substances are required to register their e-Prescribing software as well as report to the controlled drug registry each time a controlled medication is prescribed or dispensed. In order for users to access the registry, the prescriber must first create an online Health Commerce System (HCS) account. Once the HCS account is active, the prescriber can then access ROPES to register their certified electronic prescribing software application for controlled substances.
The good news is that applying for an HCS account is as easy as filling out an online form and having a New York State driver’s license (or photo ID).
Applying for an HCS Account
Requirements: New York state valid driver’s license or photo ID and New York State Education Department registered medical professional license
To apply, you will need to access the following page: https://apps.health.ny.gov/pub/top.html
After you have applied and have been granted an HCS account, you will be able to sign back in via this link: https://commerce.health.state.ny.us
You may also use the following link as a reference to see in full detail a direct guide of the application process: https://apps.health.ny.gov/pub/ctrldocs/paperless_docp.pdf
In addition to requiring an account in the Health Commerce System (HCS), if prescribers intend to order controlled substances electronically, they will also need to register their certified electronic prescribing application software with the New York State Department of Health, Bureau of Narcotic Enforcement (BNE). This is done by filling out a ROPES form online through an HCS account.
What is a ROPES form?
A ROPES form is a new online application that allows the practitioner/organization to renew their registration for the Official Prescription Program and register their certified electronic prescribing software application for controlled substances. ROPES stands for Registration for Official Prescriptions and E-prescribing Systems. Only the prescriber can access the ROPES application.
Pre-requisite Requirements for ROPES
- Prescriber must be already registered with the Official Prescription Program (OPP)
- Prescriber must have an active DEA registration
- Prescriber must have an active NY license
- Prescriber must NOT be a registered Physician Assistant (PA) – PA’s must continue to submit the OPP registration form (DOH-4329) along with the PA Authorization Form (DOH-5054) to renew their OPP registration.
Completing the ROPES Form
In order for a prescriber to fill out a ROPES form, he/she must log into his/her HCS account (outlined above) by accessing the following weblink: https://commerce.health.state.ny.us and following the next few steps:
- Select “my content†at the top of the page
- Scroll down and select “All applicationsâ€
- Scroll over and select “Râ€
- Scroll down and select “ROPES†and complete the form
The ROPES form requires that the prescriber identifies the third party audit certifying organization and the date of the third party audit. Keep in mind that it is the software vendor that must be certified not the prescriber. The software vendor will supply all necessary information about this certification to the prescriber. The ROPES form must be renewed every two (2) years in order to remain valid. The prescriber must renew their OPP registration first via the one step process prior to renewing their current ROPES registration.
Questions?
Any questions regarding the ROPES form or the process can be directed to the BNE at narcotic@health.state.ny.us or by calling 1-866-811-7957.
For prescribers utilizing DoseSpot who have questions regarding the ROPES required third party audit information, please contact DoseSpot support at 888-847-6814.
Author: Shannon K.
Sources: Practice Fusion; New York State Dental Association; New York State Department of Health
About DoseSpot
DoseSpot is a Surescripts certified e-Prescribing platform specifically designed to integrate with electronic health record, electronic dental record, practice management and telehealth software. DoseSpot is certified to e-Prescribe controlled substances and has provided simple, affordable and integratable e-Prescribing solutions to healthcare IT companies since 2009. For more information, please visit www.DoseSpot.com.
Posted: November 28th, 2016 | Author: DoseSpot | Filed under: Controlled Substances, In the News, Public Policy | Tags: Controlled Substances, DEA, Dental e-Prescribing, e-Prescribing controlled substances, e-Prescribing Integration, e-Prescribing Maine Mandate, EPCS, Healthcare Software, Maine Controlled Substance Act, Maine Controlled Substance Prescription Requirements, Maine Dose of Reality, Maine e-Prescribing Law, Maine e-Prescribing Legislation, Maine e-Prescribing Mandate, Maine e-Prescribing of Controlled Substances, Maine EPCS, Maine Opioid Law, Maine State Mandate, Mandatory e-Prescribing, Mandatory Electronic Prescribing, Opioid Epidemic, Opioids, Prescription Monitoring Program, State Mandates | No Comments »
Maine is well known for its rocky coastline, iconic lighthouses, sandy beaches, and lobster shacks. However, past the classic scenery is where you’ll find the state dealing with a crisis that others across the United States are also experiencing: the opioid epidemic.
In 2015, Maine suffered an astounding 272 drug overdose deaths, following 208 deaths of the same cause in 2014. Sadly, there is no end in sight. Maine’s Attorney General Janet Mills declared that drug overdose deaths are up 50% in 2016, with the first 6 months of the year experiencing 189 drug overdose deaths alone. What’s worse, the number of overdose-related deaths in 2016 is expected to reach a new record, surpassing those numbers of 2014 and 2015.

“Heroin addiction is devastating our communities,†Maine Governor Paul LePage said in a statement. “For many, it all started with the overprescribing of opioid pain medication.â€
As a state with the largest number of patients per capita on prescription for long-acting opioids, the news that prescribed pain medication is further fueling opioid addiction is unsettling.
This is why Maine has decided to take action.
Maine’s new statue, “An Act to Prevent Opiate Abuse by Strengthening the Controlled Substances Prescription Monitoring Program,†entails a number of rules and regulations designed to reduce the harm of over-prescribing opioids relative to the abuse and misuse of such substances. This bill, signed into law by Governor LePage, mandates a number of changes for doctors and dentists who prescribe controlled substances in Maine.
[Read: The Maine Mandate – Confronting Controlled Substances Head-On]
What changes will be implemented?
Dosing and Duration of Schedule II Medications
First, this law imposes limitations on the medication dosage, as well as the duration of a prescription, that can be prescribed to a patient. According to Gordon Smith, JD, Executive Vice President of Maine Medical Association (MMA), the original bill limited opioid prescriptions to three days for acute pain and fifteen days for chronic pain. However, this legislation will now mandate a limit of seven days for acute pain and thirty days for chronic pain on opioid prescriptions. This law goes in to effect January 1, 2017.
In terms of dosing, prescribers may not prescribe any combination of opioid medication in an aggregate amount of more than 100 Morphine Milligram Equivalents (MMEs) per day to new opioid patients (after July 29, 2016). Existing opioid patients with active prescriptions in excess of 100 MMEs per day are referred to as “Legacy Patients†and prescribers may not prescribe any combination of opioid medication in an aggregate amount of more than 300 MMEs per day from July 29, 2016 to July 1, 2017.
Prescription Monitoring Program
Maine prescribers are required to query the Prescription Monitoring Program (PMP) database prior to prescribing opiates. Although this requirement has been in place since 2005, surveys indicate that only 7-20% of Maine prescribers currently utilize the state’s PMP.
The purpose of checking this central state database is to identify patients who may be doctor shopping and minimize multiple controlled substance prescriptions for one patient. This aligns with the state’s hope of empowering healthcare providers to recognize potential substance abuse and treat patients accordingly.
PMP’s can also be most effective when linked with an e-Prescribing solution. Working together, e-Prescribing eliminates the need for paper prescriptions, thus reducing the risk of altered dispense quantities, stolen prescriptions or prescription pads, and the reselling of such prescriptions before they’re filled as a means of lessening the red flags if a patient is doctor shopping.
[Read: The Link Between PDMP’s and e-Prescribing]
Continuing Education
Via this statute, prescribers must complete three hours of continuing education every two years as a condition of prescribing opioid medications. This specific addiction training is only required if a prescriber wishes to continue prescribing opioids.
Electronic Prescribing
All opioid prescriptions must be sent electronically as of July 1, 2017.
What exceptions are part of this mandate?
The Maine Medical Association (MMA) confirms that exceptions from the law’s provisions may be granted for the following:
- Cancer Patients
- Hospice Care
- End-of-Life Care
- Palliative Care
- Patients on Medication-Assisted Therapy (MAT)
- Patients receiving medication in hospitals and nursing homes
The MMA is currently seeking an exception for burn victims as well.
Due to the supremacy clause of the U.S. Constitution, federal law takes priority over state law, therefore prescribers within the Department of Veterans Affairs (the VA) cannot be regulated by this type of legislation so long as the medication is dispensed at a VA pharmacy. Furthermore, dosage and duration limits would not apply to a prescription written for a veteran by a prescriber outside of the VA system if the prescription were filled in a VA pharmacy.
How does this bill measure up?
With this bill, Maine becomes the third state behind Minnesota and New York to require e-Prescribing and the second to require the electronic sending of a controlled substance after New York imposed a similar mandate in March of 2016. Since the implementation of New York’s mandate, total numbers of opioid analgesics prescribed fell by 78% within the first four months.
Important dates to remember:
|
7/29/2016
|
Prescribers may not prescribe any combination of opioid medication in an aggregate amount of more than 100 Morphine Milligram Equivalents (MMEs) per day to new opioid patients |
|
7/29/2016 – 7/1/2017
|
Prescribers may not prescribe any combination of opioid medication in an aggregate amount of more than 300 MMEs per day to “Legacy Patients†|
|
1/1/2017
|
Duration limitation goes into effect. All opioid prescriptions cannot exceed seven days for acute pain or thirty days for chronic pain. |
| 7/1/2017 |
All opioid prescriptions must be sent electronically |
Lastly, as part of the state’s strategy, Maine has launched Dose of Reality, a website to help educate and inform their citizens of the dangers of painkillers and where to turn for help.
Author: Lindsey W.
Sources:Â Maine Medical Association; Maine.gov; Medscape; WCSH6; Bangor Daily News
About DoseSpot
DoseSpot is a Surescripts certified e-Prescribing platform specifically designed to integrate with electronic health record, electronic dental record, practice management and telehealth software. DoseSpot is certified to e-Prescribe controlled substances and has provided simple, affordable and integratable e-Prescribing solutions to healthcare IT companies since 2009. For more information, please visit www.DoseSpot.com.
Posted: October 27th, 2016 | Author: Shauna | Filed under: Basics, Controlled Substances, In the News, Public Policy, Security, Standards | Tags: Controlled Substances, DEA, DoseSpot, e-Prescribing, e-Prescribing controlled substances, e-Prescribing Integration, e-Prescribing Software, electronic prescribing, Healthcare Software, Opioid Epidemic, Opioids, Patient Engagement, PDMP, PMP, Prescription Drug Monitoring Program, Prescription Monitoring Program, State Mandates, trends, Value Based Care | No Comments »

On par with our last post, the widespread media attention and devastating losses associated with our nation’s current opioid epidemic has sparked certain state legislatures to regulate and improve providers’ prescribing habits for prescription painkillers.
With good intentions in tow, some rulings seem to lack readily available solutions that are proven to curb this crisis. However, they do realize that their recent proposals do not mark the end of this uphill battle, rather multifaceted solutions need to be in place to truly, and successfully, overcome this epidemic.
[Read: Overdose Awareness – The Time to Stand Together is Now]
Here are three states that have recently proposed rulings on how opioids should be prescribed:
Vermont
Coined as a “cutting-edge†approach to overcoming the opioid crisis, Governor Peter Schumlin announced proposed limits on the number of opioid medications that could be prescribed.
Like every other state, Vermont has seen an incredible increase in deaths related to opioid and heroin overdose in recent years and Governor Schumlin is no longer sitting on the sidelines.
Earlier this year, he approached both the FDA and pharmaceutical industry in his State of the State address claiming that OxyContin “lit the match that ignited America’s opiate and heroin addiction crisis,†and that the booming American opiate industry knows no shame, an outcry after the FDA approved OxyContin for children a few months ago.
The proposed ruling states that the severity and duration of pain will determine the specific limit for a prescription of opioids. For example, a minor procedure with moderate pain would be limited to 9-12 opioid pills and the amount would increase based on the procedure performed and the level of pain a patient claims. The ruling would also require providers to discuss risks, provide an education sheet to the patient and receive an informed consent for all first-time opioid prescriptions.
The Green Mountain State’s Governor believes that limiting the number of opioid pills prescribed would be an effective way to reduce addiction, yet some folks believe the ruling would only encourage patients to seek illicit drugs elsewhere if they cannot receive pain medication through their provider.
This does make sense considering many former and current heroin abusers have stated that their addiction started from a prescription and when the pill bottle ran out, they were left seeking these drugs on the streets, which have proven to be very, if not more, dangerous than the prescription.
However, the intent of the Governor’s ruling is to prevent addiction from ever happening in the first place. His ruling is specific to cases of acute pain, therefore changing the over-prescribing habits and learned behavior of utilizing opioids as first-line therapy; habits that ensued in large part due to incentives, the surge of pharmaceutical marketing tactics and claims that painkillers were not addictive.
[Read: How Costly Are Prescription Pain Meds?]
New Jersey
With the rate of drug overdose deaths on the rise by 137% since 2000, New Jersey is another state to recently propose new regulations on how and to whom opioids are prescribed.
New Jersey, much like many other states, believes that prevention is key when fighting this crisis and they couldn’t be more correct. Unfortunately, several barriers often occur when seeking appropriate treatment after a patient becomes addicted, (for example, providers are limited to certain amounts for which they can administer reversal drugs), and therefore why not PREVENT addiction, rather than simply TREAT addiction when at many times, it’s too late?
Senator Raymond Lesniak has introduced a bill that would put restrictions on health insurance coverage for opioid medications, while also requiring prescribers to first consider alternative pain-management treatments, follow federal prescribing guidelines and explain the risk of addiction with such substances to their patients before prescribing. Furthermore, providers will need to complete several steps before receiving approval of an opioid prescription. These steps include providing a patient’s medical history, conducting a physical exam and developing an appropriate medical plan for treating a patient’s pain.
While new rulings in place can certainly shift this epidemic, Angela Valente, the executive director of the Partnership for a Drug-Free New Jersey, said it best:
“Awareness and education is the key factor in preventing the abuse of opiates—everyone must have a role in reversing this epidemic, including lawmakers, parents, coaches, educators, and yes, even doctors and dentists.†– Angela Valente
Dr. Andrew Kolodny, executive director of Physicians Responsible for Opioid Prescribing, further backs Valente’s point while also motioning that the medical community has been prescribing too aggressively.
[Read: The Opioid Epidemic: Are Dentists the Black Sheep?]
Pennsylvania
Unfortunately, Pennsylvania experienced 3,500 deaths last year as a result from drug overdose, one of the highest overdose rates in the nation.
The state has had a Prescription Drug Monitoring Program for quite a few years now, however it wasn’t functional until August 2016, when their new program was officially rolled out. Pennsylvania requires providers to query the state’s prescription drug database the first time they prescribe a controlled substance to a patient or if they have reason to believe that the patient is doctor shopping.
Governor Tom Wolf addressed other initiatives underway including requiring providers to query the database EACH time they prescribe opioids, updating medical school curriculum and continuing education, changes to the process of pain care to lower inappropriate use of opioids, and improved screening, referral and treatment for addiction.
What’s bothersome in Pennsylvania, is the method in which these substances have to be prescribed. The Pennsylvania Controlled Substance Act requires narcotic prescriptions to be handwritten on paper prescription pads, yet every other substance can be electronically prescribed. This allows the risk of written prescriptions being lost, stolen, or sold. Luckily, Senator Richard Alloway intends to introduce this measure before the legislative session’s end.
It’s promising to see how the above states are utilizing their state’s Prescription Drug Monitoring Program, or PDMP. All three require their prescribers to query the affiliated state database, however the parameters in which, or how often, they check varies.
While said efforts are better than no effort at all and states are starting to fully understand the need for multifaceted solutions in order to overcome this epidemic, one key solution is missing. E-Prescribing.
[Read: The Link Between PDMP’s and e-Prescribing]
How does e-Prescribing help combat this epidemic?
- e-Prescribing diminishes the possibilities of duplicate or lost prescriptions since the prescription is sent directly to the patient’s pharmacy
- A patient will no longer have a paper prescription where the dispense quantity can be altered
- Prescribers will have access to a patient’s medication history, therefore they can determine if a patient is “doctor shopping†or has a history of substance abuse
To learn how to incorporate e-Prescribing as a solution to the opioid epidemic, schedule a meeting with DoseSpot today.
Sources:Â NY Times; Boston.com; ABC News; Press of Atlantic City; PennLive
About DoseSpot
DoseSpot is a Surescriptsâ„¢ certified e-Prescribing platform specifically designed to integrate with electronic health record, electronic dental record, practice management and telehealth software. DoseSpot is certified to e-Prescribe controlled substances and has provided simple, affordable and integratable e-Prescribing solutions to healthcare IT companies since 2009. For more information, please visit www.DoseSpot.com.
Posted: September 15th, 2016 | Author: Shauna | Filed under: Basics, Controlled Substances, Public Policy | Tags: Boston Opioid Hack-a-Thon, Controlled Substances, e-Prescribing, e-Prescribing controlled substances, healthIT, Opioid Epidemic, Opioids, Patient Engagement, trends | No Comments »
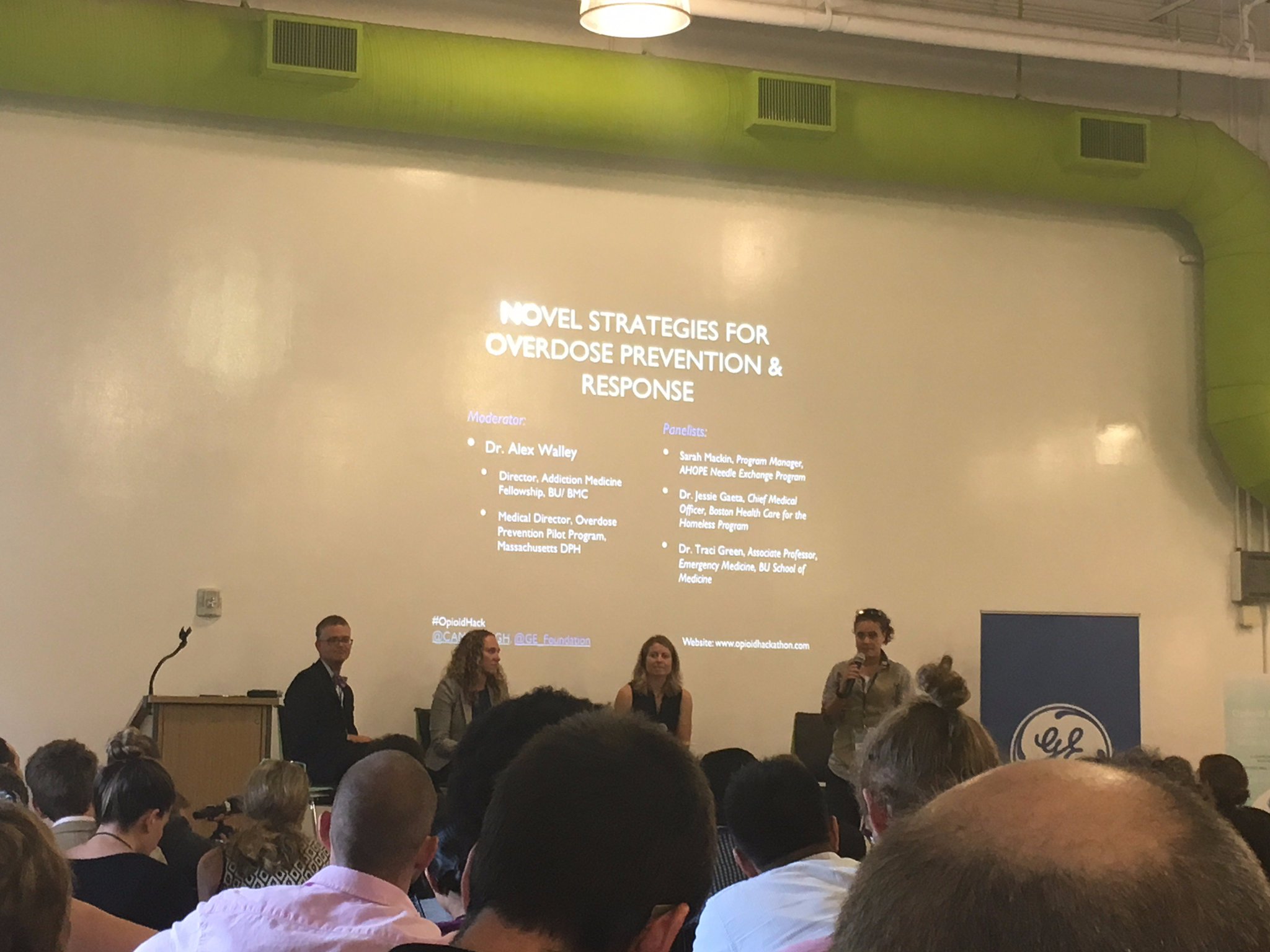
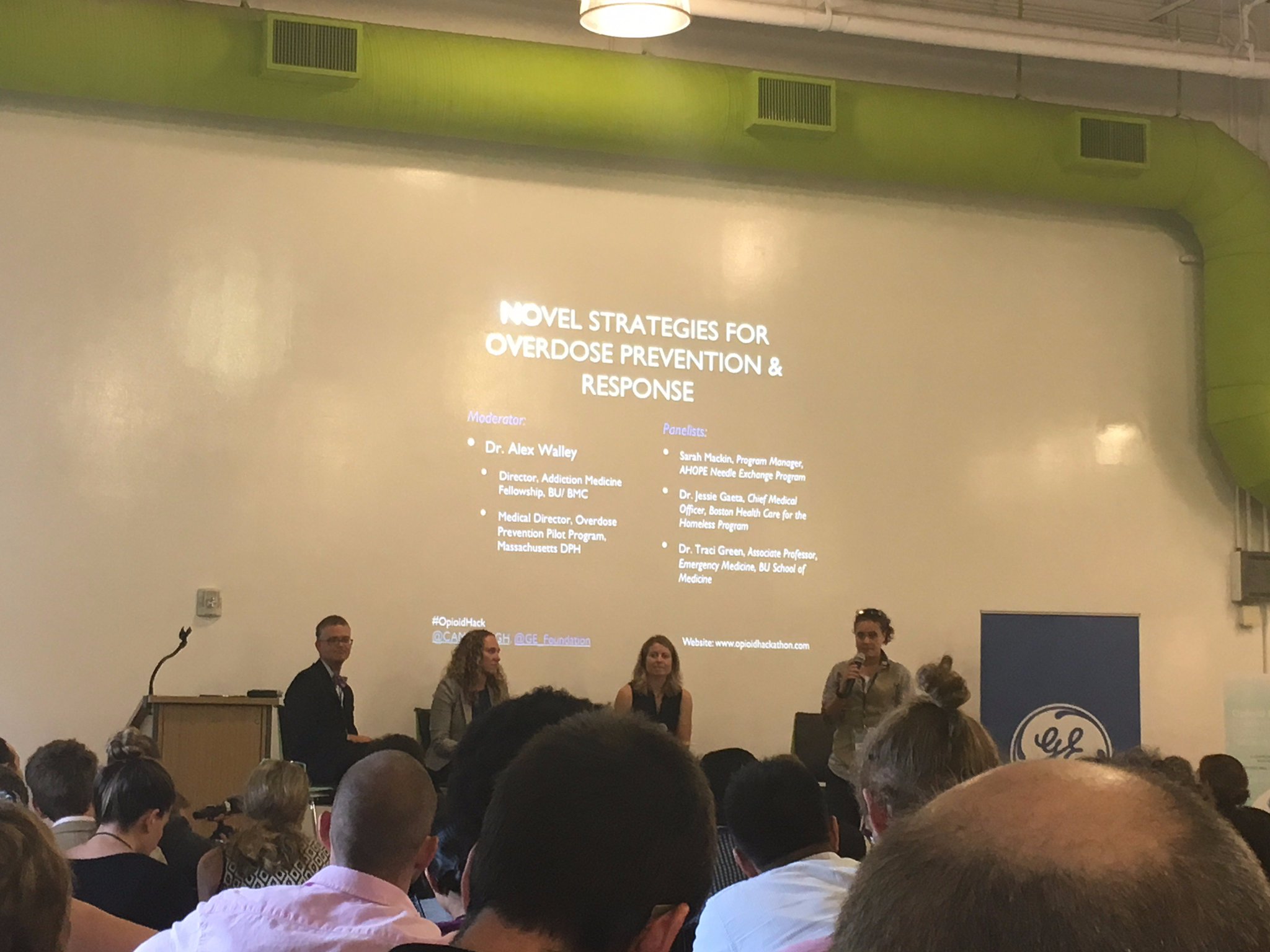
Recently, DoseSpot was fortunate to attend Boston’s first ever opioid epidemic hack-a-thon to hear from key opinion leaders in an effort to pitch solutions on how to combat the country’s rising opioid epidemic. Sponsored by the GE Foundation and Massachusetts General Hospital (MGH), the event was comprised of like-minded individuals from all walks of life and specialties, many whom normally wouldn’t sit side by side in the same room until this specific event brought them together. Attendees were given the opportunity to innovate, think differently about this issue and further realize that a significant change is needed in order to tackle this fatal crisis currently grappling our nation.
After attending the summit, the message was clear: we can no longer sit back and believe that there is a one-stop solution. Collective efforts must be put in place and educating and incorporating all components of the healthcare system is imperative to its success.
Here are DoseSpot’s 3 takeaways from the summit:
Opioid addiction does not discriminate
Athletes, politicians, police officers, clinicians, mothers, fathers, siblings, children. Regardless of one’s socioeconomic status, opioid abuse and addiction can affect anyone. In MA alone, there are 4 deaths per day due to opioid overdose and in 2012 there were enough opioid prescriptions to give every American adult their own bottle of pills. However, beyond these statistics are the stories and these courageous stories rang loudly throughout the entire event.
Treat opioid addiction just like any other chronic illness
The stigma associated with addiction often deters people from receiving the treatment they need, and worse, sometimes that stigma is put in place by the very people meant to help them. As many of the speakers at the summit expressed, overcoming stigma should be of utmost priority and addiction should be treated in an effective, mainstream way just like any other condition. Addiction is not a choice; it is a disease.
There needs to be multifaceted solutions to tackle this complex problem
One panelist pointed out that the nation is not thinking big enough or differently enough. Clinicians and healthcare professionals may have blinders on when treating patients, but “one size does not fit all†should be the mantra that everyone utilizes when evaluating their treatment approach. A provider shouldn’t refer to themselves as a one treatment option provider, but utilize all best practices available. As Governor Baker asked, “Wouldn’t you be a better clinician if you expanded your knowledge through a variety of options and techniques?†This includes big data, analytics, e-Prescribing, Medication Assisted Therapy (MAT) and much, much more.
Sources:Â WBUR; Boston Globe; The Daily Free Press; Boston Business Journal
About DoseSpot
DoseSpot is a Surescripts certified e-Prescribing platform specifically designed to integrate with electronic health record, electronic dental record, practice management and telehealth software. DoseSpot is certified to e-Prescribe controlled substances and has provided simple, affordable and integratable e-Prescribing solutions to healthcare IT companies since 2009. For more information, please visit www.DoseSpot.com.
Posted: August 31st, 2016 | Author: Shauna | Filed under: Basics, Controlled Substances, In the News, Public Policy | Tags: CBS News, CNN, Controlled Substances, e-Prescribing, e-Prescribing of Controlled Substances, EPCS, International Overdose Awareness Day, Opioid Epidemic, Opioid Prescriptions, Opioids, Overdose Awareness Day, PDMPs, Shatterproof, State Mandates, Time Magazine | No Comments »
International Overdose Awareness Day
To some, this day may not mean much, but to others, it is a day to commemorate and remember loved ones that we lost as a result of overdose. Unfortunately, these fatal occurrences are in large part due to a horrible, stigmatized and chronic illness: addiction.
While there has been widespread media attention for how addiction “should†be categorized as outlined in the latest New York Times article, addiction, specifically with opioids, is still viewed as a moral failing, a flaw, even. The associated stigma often deters patients from receiving proper rehabilitation treatment and even if they do seek treatment, the government currently limits the number of patients a single provider may treat with drugs such as buprenorphine or methadone, which are both proven to reduce cravings and save lives. This leads to many patients relapsing.
Physicians, internists, and dentists are collectively responsible for providing 81.6% of opioid prescriptions in the United States and because of this, they have a very unique role in mitigating the impact of this opioid epidemic. Opioid addiction often starts at the hands of healthcare professionals simply trying to do their job, prescribing pain medications to relieve their patients of painful woes, especially during post-operative recovery.
While many prescriptions are meant for initial, short-term treatment, some doctors and dentists authorize refills time and time again because they want to help patients whom claim that they are still in pain. However, when the pill bottle and refills run out, these patients are left high and dry; looking for alternatives to create that euphoric escape they’ve become so accustomed to. This could mean an endless search of several different doctors to prescribe more substances (also known as doctor shopping), purchasing pills on the black market, or worse, turning to heroin as a cheaper and more readily available alternative.
As the Surgeon General, Dr. Vivek Murthy, reiterates in his recent letter to all of America’s doctors, many prescribers don’t realize how dangerous the drugs can be, or even how addictive they are because many were incorrectly taught that opioids are not addictive when prescribed for legitimate pain. Dr. Murthy further points out that overdose deaths from opioids have quadrupled since 1999 and pain medication prescriptions have risen to the point that there’s enough for every American adult to have their own bottle of pills. It’s a fair statement that the majority of clinicians do not enter the healthcare industry with intent to harm their patients, yet it’s also fair to say that lack of proper education has further fueled these prescribing patterns.
So, who’s to blame here? Is it the prescribers? The pharmaceutical companies’ aggressive marketing tactics in the 1990’s? Learned behaviors? The demands and expectations from patients?
The truth of the matter is: no one is to blame. Blaming only diverts the necessary explication of collectively coming together as a nation to address this epidemic. The imperative solution is education.
Dr. Murthy also addresses in his letter that now is the time for clinicians to properly educate themselves on how to treat pain safely and effectively and screen patients for opioid use disorder and provide them with helpful resources and evidence-based treatment options. Furthermore, to shape how the rest of the country sees addiction, clinicians should shamelessly speak about it and start treating it as a chronic illness.
As a part of this ongoing education initiative, DoseSpot will be hosting a webinar in regards to the opioid epidemic that will include helpful tips and resources to stay ahead of this crisis. Stay tuned for more details.
Sources: Time; CNN; Time; Aetna; Surgeon General Letter; Shatterproof; CBS News
About DoseSpot:
DoseSpot is a Surescripts certified e-Prescribing platform specifically designed to integrate with electronic health record, electronic dental record, practice management and telehealth software. DoseSpot is certified to e-Prescribe controlled substances and has provided simple, affordable and integratable e-Prescribing solutions to healthcare IT companies since 2009. For more information, please visit http://www.DoseSpot.com.
Posted: July 19th, 2016 | Author: Shauna | Filed under: Basics, In the News, Public Policy, Telehealth | Tags: digital adoption, digital health, DoseSpot, e-Prescribing, electronic prescribing, healthcare technology, Medicaid, Medicare, NEJM, New England Journal of Medicine, telehealth, telemedicine | No Comments »

A study recently published by The New England Journal of Medicine stated that telehealth is positioned to revolutionize medical care. It’s fair to say that technologies are making a lot of things possible that wouldn’t have happened even a few years ago, but it’s also fair to say that this new age of telemedicine poses new risks and a few hurdles to overcome for the healthcare industry, providers, and patients alike.
One limitation that the industry is currently experiencing is the adoption of reimbursement for medical delivery systems by payers across the country, specifically the lack of coverage and “unequal†treatment of receiving care via technological advances. Luckily, certain states have put telehealth parity laws into place, thus requiring coverage and reimbursement for telehealth under private insurance, Medicaid, and workers compensation as though services were provided in person. Medicare, on the other hand, seems to be last to join the party which makes sense considering the population it serves.
Want to learn more? Download our free telehealth whitepaper!
Throughout the article, the biggest issue rings loudly: the digital divide between the industry and the populations they serve, whether that be the elderly, lower income individuals, or the less educated. These groups are less likely to have the means to participate in telehealth options. No computer or smartphone = no digital health adoption.
While there are a few bumps in the road, telehealth does serve up some benefits as well:
- Doctors across several specialties are easily accessible for patients. This helps individuals with time constraints, lack of transportation or means to visit a doctor, and includes those whom have chronic diseases that need to be monitored closely and more frequently.
- Telehealth is cost-effective. What one may pay toward their deductible or out-of-pocket maximum for an in-office visit is undoubtedly lower than an e-visit which can typically be found for $50 or less.
- E-visits will contribute to less hospital readmissions, therefore reducing overall healthcare and drug spend which is astronomical in this country.
Ultimately, telehealth is meant to be an extension of the provider’s office, not a replacement. It will enable medical professionals to meet the growing burden of chronic disease, while enhancing the patient-centric, value-based care model the United States is currently trying to implement.
What do you think of this shift to digital health? Exciting or nerve-wracking? Share your thoughts with me below!
Sources: The New England Journal of Medicine
About DoseSpot
DoseSpot is a Surescripts certified e-Prescribing platform specifically designed to integrate with electronic health record, electronic dental record, practice management and telehealth software. DoseSpot is certified to e-Prescribe controlled substances and has provided simple, affordable and integratable e-Prescribing solutions to healthcare IT companies since 2009. For more information, please visit http://www.DoseSpot.com.


 Follow
Follow